St. Luke's Health joins CommonSpirit.org soon! Enjoy a seamless, patient-centered digital experience. Learn more

Diabetes & Endocrinology — Baylor St. Luke's Medical Center
Baylor St. Luke’s Medical Center is an internationally recognized leader in innovation, research and clinical excellence that has given rise to breakthroughs in cardiovascular care, neuroscience, oncology, transplantation, and more. Our team’s efforts have led to the creation of many research programs and initiatives to develop advanced treatments found nowhere else in the world.
Our strong alliance with Baylor College of Medicine allows us to bring our patients a powerful network of care unlike any other. Our collaboration is focused on increasing access to care through a growing network of leading specialists and revolutionizing healthcare to save lives and improve the health of the communities we serve.
Baylor St. Luke’s Medical Center is also the first hospital in Texas and the Southwest designated a Magnet® hospital for Nursing Excellence by the American Nurses Credentialing Center, receiving the award six consecutive times.
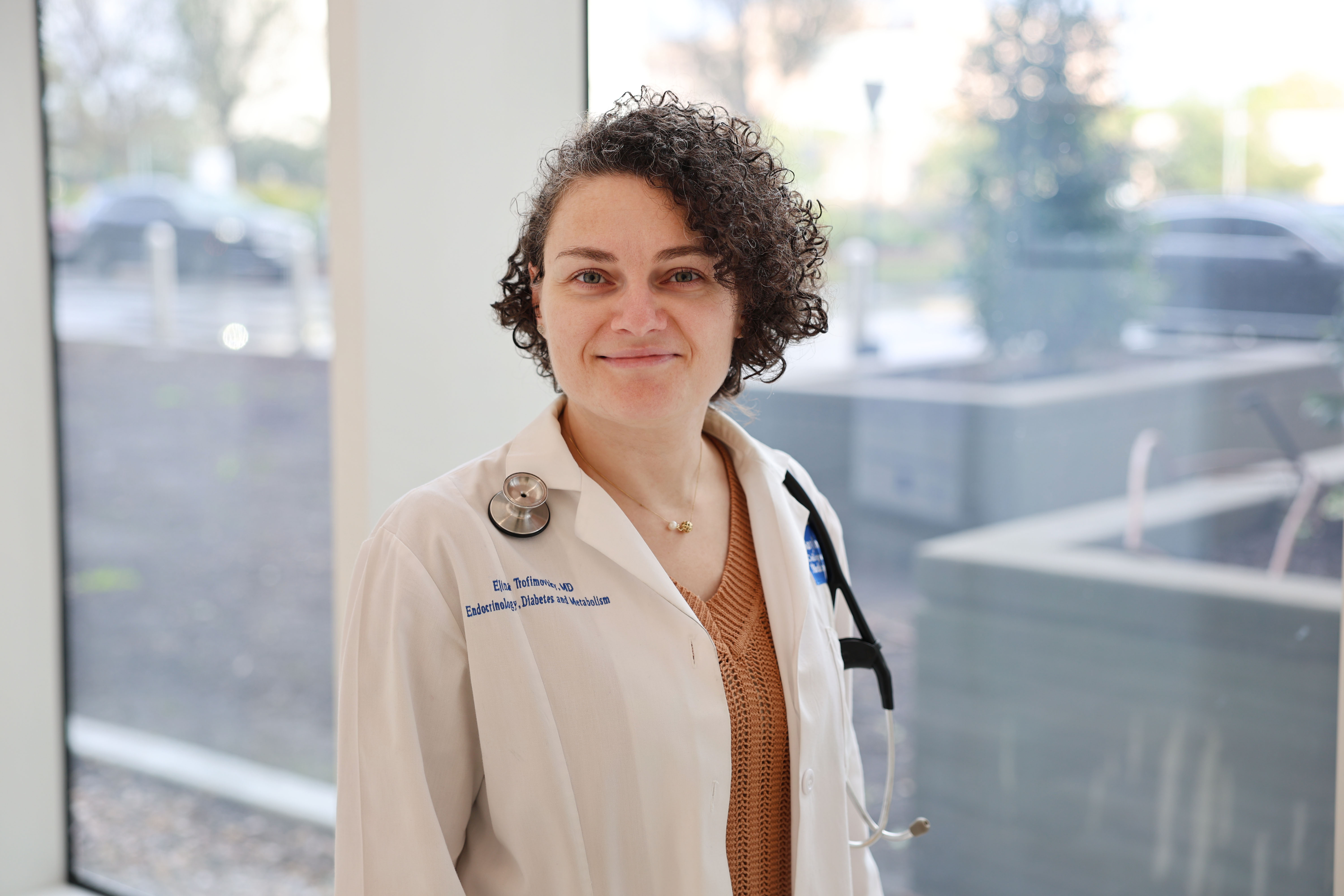
For people with diabetes who are struggling with depression, there are effective and better treatment approaches to help patients manage and mitigate their symptoms.
Dr. Elina Trofimovsky, an endocrinologist at Baylor College of Medicine, mainly works with patients who have diabetes and has seen first-hand how diabetes distress and depression negatively impact patients’ motivation and self-care.
Diabetes is a chronic disease in which the pancreas is unable to produce enough insulin leading to elevated blood sugar levels. Diabetes can have deleterious effects on the kidneys, eyes, and circulatory, digestive and nervous systems. Symptoms include excessive thirst and urination, excessive hunger, weight loss, blurry vision, and recurrent infections.
Living with diabetes can be overwhelming for many patients, especially those who are on insulin multiple times a day. People with diabetes are much more likely to have depression than those without. Symptoms of depression can range from overeating to a loss of appetite, sleeping too little or too much, to excessive fatigue and suicidal thoughts.
Dr. Trofimovsky counsels her patients to see their physician regularly and work with a dietitian or diabetes educator to create small, realistic goals to improve their diets and self-care routine. Patients should also work with a psychiatrist and psychologist to develop a treatment plan, enlist the help of family or friends if available, and seek out support groups.
Baylor St. Luke’s Medical Center (BSLMC) is a leader in the fight against diabetes. And at the forefront is Dr. Mandeep Bajaj, one of the nation’s most recognized specialists and researchers in type 2 diabetes, its causes, treatments, management, and prevention. Dr. Bajaj, who heads BSLMC’s Endocrinology Section and is the Medical Director of BSLMC’s Diabetes Program and Baylor Medicine Endocrinology and Diabetes, has now stepped into the role of President of Medicine and Science of the American Diabetes Association (ADA). His one-year board appointment started in January 2024.
Dr. Bajaj, who came to Baylor College of Medicine in 2006, has been in practice for over 25 years. A reputed clinical and translational researcher in obesity and type 2 diabetes, Dr. Bajaj has over one hundred publications. His patient-oriented research work has delineated the metabolic and molecular mechanisms of insulin resistance in the pathogenesis of type 2 diabetes.
In his new role as ADA’s President-elect, Dr. Bajaj emphasizes the organization’s efforts to educate the public about diabetes and its risk factors. Currently, more than 37 million people in the US have been diagnosed with diabetes and more than 90 million people are pre-diabetic, putting them at higher risk of developing the disease, which also can lead to other serious health issues like heart and kidney disease, stroke, impaired vision and neurological conditions.
Dr. Bajaj is also deeply committed to championing health equity for all patients.
“The important step in ensuring health equity is making sure underserved patients have access to education, routine screenings and the newest treatments through both primary care doctors and specialists,” said Dr. Bajaj. Bringing down the cost of care is also critical to effective disease management. Dr. Bajaj notes the organization’s leading role advocating for affordable insulin which led to the historic enactment in July of 2023 of a $35/month price cap on the cost of insulin for diabetes patients on Medicare.
A medical graduate of the All-India Institute of Medical Sciences in New Delhi, Dr. Bajaj is the son of a prominent endocrinologist in India who followed in his father’s footsteps. He received his fellowship training in endocrinology and diabetes at the Joslin Diabetes Center in Boston.
Dr. Bajaj has been awarded the Master Clinician Lifetime Award as well as the Fulbright & Jaworski Faculty Excellence Teaching Award by Baylor College of Medicine. He is currently the editor-in-chief of British Medical Journal (BMJ), Open Diabetes Research and Care, published jointly by the ADA and the BMJ Group.
During his tenure as President of the ADA, Dr. Bajaj will continue to press for more federal funding to support research into the causes and prevention of diabetes, and use his leadership platform at Baylor to champion equitable care for all patients who have diabetes or are at risk of developing the disease.
“Maintaining a healthy lifestyle,” noted Dr. Bajaj, “is one of the best preventative measures people can take to reduce their risk of developing this life-altering disease.”

Mandeep Bajaj, MD
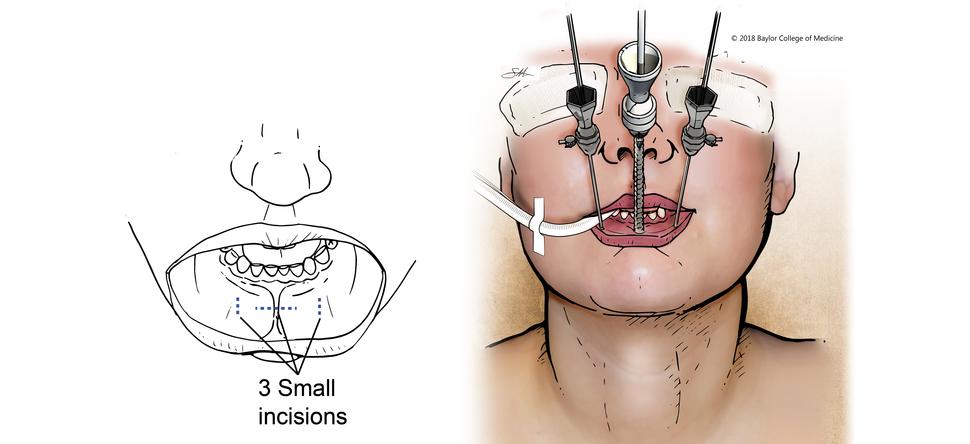
One of the most exciting developments in thyroid and parathyroid care in the last decade is an innovative surgical procedure that allows surgeons to remove the thyroid and parathyroid without leaving a scar or damaging the voice.
Baylor St. Luke's is the only hospital in the state of Texas, and one of just five high-volume centers in the U.S., to offer the transoral endoscopic thyroidectomy vestibular approach (TOETVA) that allows for a scarless thyroid and parathyroid removal.
With an incision length of 2 cm or less, TOETVA is a minimally invasive procedure where the surgeon goes through the inner lip to remove the thyroid, which leaves no sign of external scarring. The procedure can also protect the parathyroid glands (if it doesn’t require removal) as an additional benefit.
Thyroid cancer is treatable with surgery, but traditional approaches have adverse side effects such as vocal changes and scarring. Now, the minimally invasive TOETVA allows the surgeon to go through an incision of 2 cm or less on the inner lip to remove the thyroid and leave no sign of external scarring. The procedure can also protect the parathyroid glands (should their removal not be required).
Patient satisfaction after the operation is extremely high.
Studies led by Baylor St. Luke's have determined that more than half of patients are eligible for TOETVA. Patient satisfaction after the operation is extremely high.
The Thyroid and Parathyroid Center at the Dan L Duncan Comprehensive Cancer Center is one of the only fully integrated multidisciplinary clinics of its kind in Texas. Combining endocrinologists and endocrine surgeons in the same clinic ensures fluid communication, faster diagnosis times, and prompt operation availability. This combined with surgical expertise that results in optimized operating times—meaning less time under general anesthesia—and even same-day discharges create a patient experience that is unrivaled in the state of Texas. The Thyroid and Parathyroid multidisciplinary team at Baylor St. Luke’s Medical Center is comprised of experts in complex cases for both benign and malignant thyroid, parathyroid, and adrenal disorders and has complication rates well below national gold standards.

Cynthia Doyle was familiar with papillary thyroid cancer because it had affected several members of her family before. She knew her cancer was treatable with surgery, but she had witnessed the side effects. She wanted to avoid trouble with her voice and the scar on her throat so she began to hunt for scarless thyroid surgery.
She soon discovered Dr. Raymon Grogan, section chief of endocrine surgery at Baylor St. Luke’s Medical Center. He is one of the only doctors in the nation who performs transoral thyroidectomy, or TOETVA—a scarless thyroid surgery that allows for the safe and total removal of the thyroid or parathyroid glands without any external scarring to the neck. Shortly after surgery, Cynthia was informed her cancer was entirely removed with negative surgical margins.

Baylor St. Luke’s Medical Center is one of five high-volume centers in the United States, to offer the transoral endoscopic thyroidectomy vestibular approach (TOETVA) that allows for a scarless thyroid and parathyroid removal. This is one of the most innovative and unique operations in all of surgery and one of the most exciting developments in thyroid and parathyroid care in the last decade.
Dr. Raymon Grogan, endocrine surgery section chief at Baylor St. Luke’s Medical Center and associate professor at Baylor College of Medicine, has completed over 200 TOETVA procedures. Baylor St. Luke’s Medical Center is one of three high-volume academic thyroid- and parathyroid-focused surgical practices in the U.S. that studied 1,000 consecutive thyroid and parathyroid operations, determining more than half to be eligible for transoral endoscopic thyroidectomy vestibular approach (TOETVA).
“The most common scarless thyroid and parathyroid techniques currently used in the United States are transoral endoscopic thyroidectomy vestibular approach for thyroidectomy (TOETVA) and transoral endoscopic parathyroidectomy vestibular approach for parathyroidectomy (TOEPVA).” - Raymon Grogan, MD
With the incision length of 2 cm or less, TOETVA is considered minimally invasive or remote access. The procedure is very unique because the surgeon goes through the inner lip to remove the thyroid, which leaves no sign of external scarring. The procedure also protects the parathyroid as an additional benefit. Patient satisfaction after the operation is extremely high.

Raymon Grogan, MD
The Section of Endocrinology, Diabetes and Metabolism at Baylor College of Medicine supports a robust biomedical research base. The Diabetes Research Center explores a vast range of diseases and conditions but focuses its efforts in four key areas: diabetes, metabolism, and nutrition research; the area of diabetes pathobiology and pathophysiology; the area of molecular lipid, glucose, and energy homeostasis; and the area of molecular endocrinology.
One additional area of research is in thyroid cancer. Almost half the population in the United States has a nodule in the thyroid, however when evaluating these nodules for cancer nearly 20% of fine needle aspiration (FNA) biopsies are found to be indeterminate in diagnosis based on cytological evaluation. Led by Dr. James Suliburk, endocrine surgeon at Baylor St. Luke’s Medical Center and associate professor and chief of endocrine surgery at Baylor College of Medicine, a new alternative uses metabolic analysis by desorption electrospray ionization mass spectrometry (DESI-MS) imaging for direct analysis and diagnosis of follicular cell-deprived neoplasia tissues and FNA biopsies. During the latest clinical study, 68 patients were tested, and the new MassSpec Pen returned a false positive only 1 time out of 10.
“With this next-generation test, we can provide thyroid cancer diagnoses faster and with more precision than current techniques.” - James Suliburk, MD
The next step is a two-year validation study including over 1,000 patients in the U.S., Brazil, and Australia.

James W. Suliburk, MD, FACS
The largest and busiest in Texas, the Pituitary Center cares for all pituitary-related disorders, including tumors of the pituitary and sellar region. The multidisciplinary team approach includes both endocrinologists and neurosurgeons working to develop and place patients on clinical trials aimed at establishing new therapies for pituitary tumors.
Led by Dr. Ali Jalali, neurosurgeon at Baylor St. Luke’s Medical Center, and Dr. Bahar Force, endocrinologist at Baylor St. Luke’s Medical Center and assistant professor at Baylor College of Medicine, the team remains experts in minimally invasive endoscopic pituitary surgery and non-surgical treatment, including CyberKnife®.

Dr. Ali Jalali