St. Luke's Health joins CommonSpirit.org soon! Enjoy a seamless, patient-centered digital experience. Learn more

Urology — Baylor St. Luke's Medical Center
Baylor St. Luke’s Medical Center is an internationally recognized leader in innovation, research and clinical excellence that has given rise to breakthroughs in cardiovascular care, neuroscience, oncology, transplantation, and more. Our team’s efforts have led to the creation of many research programs and initiatives to develop advanced treatments found nowhere else in the world.
Our strong alliance with Baylor College of Medicine allows us to bring our patients a powerful network of care unlike any other. Our collaboration is focused on increasing access to care through a growing network of leading specialists and revolutionizing healthcare to save lives and improve the health of the communities we serve.
Baylor St. Luke’s Medical Center is also the first hospital in Texas and the Southwest designated a Magnet® hospital for Nursing Excellence by the American Nurses Credentialing Center, receiving the award six consecutive times.
In collaboration with the Dan L Duncan Comprehensive Cancer Center and Baylor College of Medicine, Baylor St. Luke’s carries out innovative translational research that provides patients with cutting-edge clinical options.
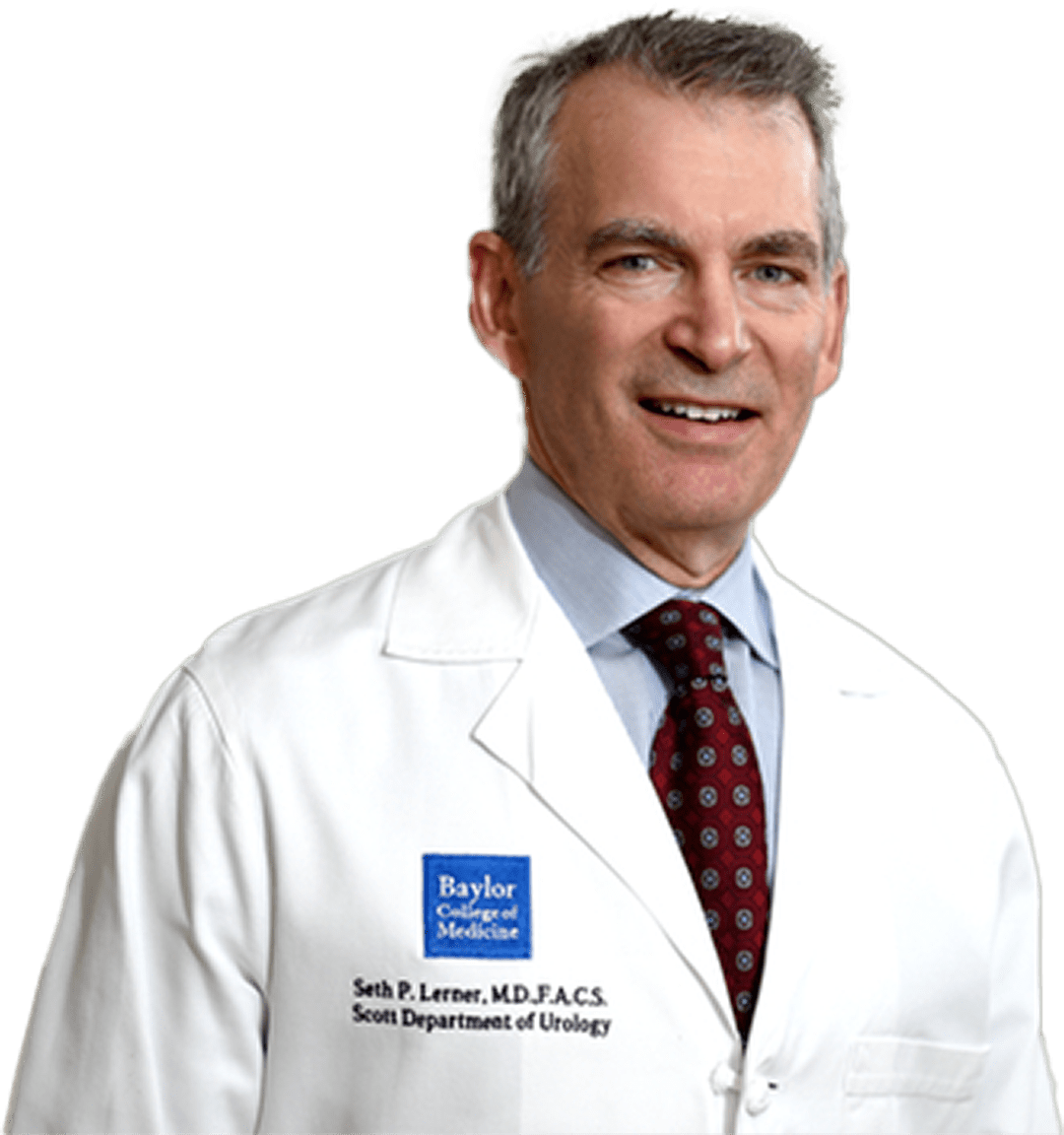
Dr. Lerner and his team published the final results of the SWOG S1011 clinical trial in the New England Journal of Medicine on Oct. 3. This trial tested if a more extensive lymph node dissection performed at the time of radical cystectomy would lead to improved disease-free and overall survival within six years following surgery. The results of this trial clearly show that there is no advantage to the more extensive surgery, changing the standard of care to include the lymph nodes in the pelvis only.
In addition to its findings on the effectiveness of extensive lymph node dissection, the Lerner Lab has completed running the NanoString assay on 313 RNA samples from the S1011 trial. NanoString is an advanced technology that enables the reliable and reproducible assessment of the expression of up to 800 genes or 228 gene fusions in 12 samples in a single assay. This high throughput method will streamline the determination of the subtype of a patient’s cancer. Dr. Lerner’s team demonstrated that this assay reliably identifies one of five molecular subtypes using a fraction of the RNA required for whole transcriptome RNA sequencing. The analysis was finalized in November. The lab will integrate these data and the NanoString subtype calls to test whether molecular subtypes can predict outcomes for patients undergoing radical cystectomy.
The Scott Department of Urology's Division of Male Reproductive Medicine and Surgery is at the forefront of advancing surgical techniques and medical practices to enhance men's health and overall well-being. This year, Dr. Blair Stocks, M.D., Ph.D., joined the faculty after completing his residency and fellowship in male reproductive medicine and surgery. He joins esteemed colleagues Dr. Larry Lipshultz and Dr. Mohit Khera as part of our dedicated men’s health and reproduction team.
Recently, Dr. Mohit Khera presented the results of the TRAVERSE clinical trial, the largest randomized placebo-controlled trial on testosterone therapy in men. The study concluded that testosterone does not increase the risk of cardiovascular events. Additionally, a sub-study revealed that while testosterone did not significantly improve erectile dysfunction, it did enhance libido, with effects lasting up to two years.
Dr. Larry Lipshultz and Dr. Blair Stocks are pioneering the use of Oxford Nanopore’s technology for native DNA methylation sequencing to develop an assay for detecting cell-free DNA (cfDNA) in seminal plasma. This method aims to assist men with non-obstructive azoospermia (NOA). Traditional retrieval methods, like microdissection testicular sperm extraction (mTESE), are invasive, expensive, and have a 50% failure rate. This non-invasive technique could predict the presence of sperm, providing valuable information to clinicians and patients before considering invasive surgery.
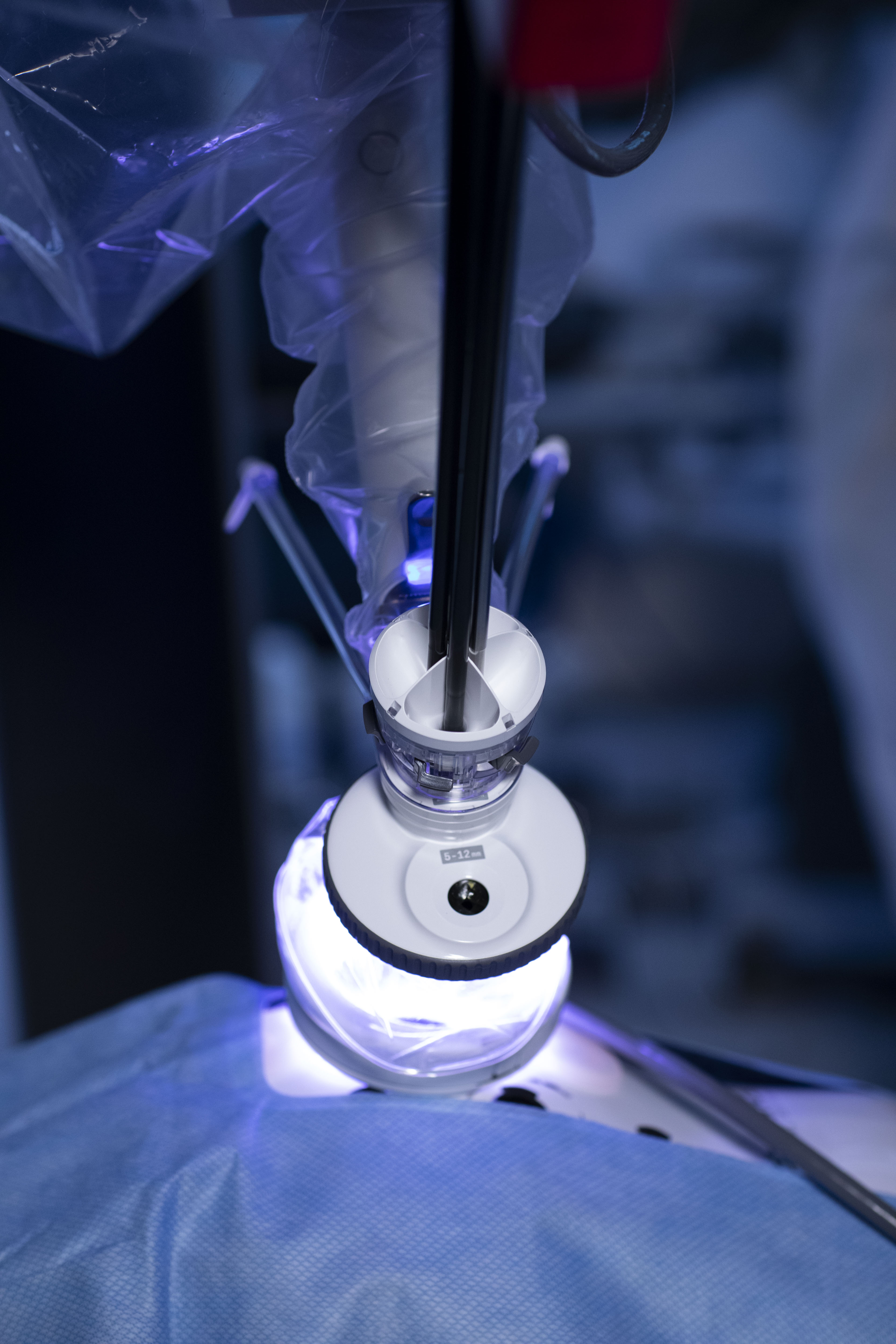
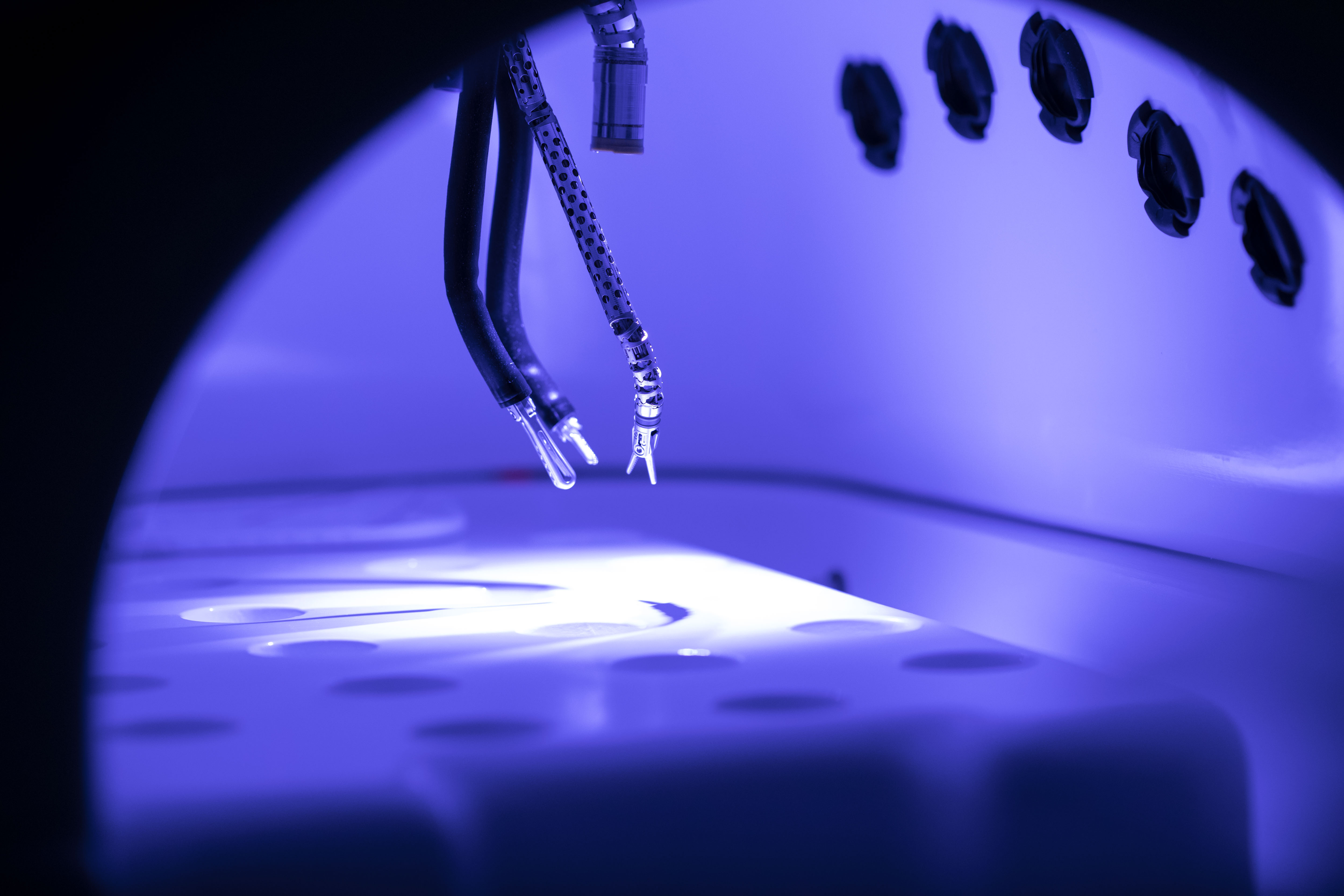
Urologists at Baylor St. Luke’s are leveraging innovative technologies to improve the treatment of bladder conditions. These technologies are enhancing the accuracy of diagnoses and the effectiveness of treatments, leading to better patient outcomes and improved quality of life.
Christopher Smith, M.D., M.S.S. M.B.A., is testing the usage of neurostimulation to treat patients living with urgency urinary incontinence who haven’t had success through behavior changes, pelvic floor therapy, or medicinal therapies. This five-year study is assessing the safety and effectiveness of the FDA-approved eCoin Peripheral Neurostimulator System. The device is implanted under the skin of the ankle to stimulate the tibial nerve, allowing feeling and movement to parts of the leg and foot. This nerve also influences the nerves controlling the bladder. In a previous clinical study with 133 participants, eCoin displayed a 50 percent or greater reduction in urgency urinary incontinence episodes up to one year after activation in 68 percent of patients.
For patients living with interstitial cystitis, visceral pain is the most common type of pain associated with the disease. A phase 2 randomized, double-blind, placebo-controlled, adaptive study is evaluating the efficacy of a compound called Linaclotide that can be used to relieve visceral pain in patients suffering from bladder and gastrointestinal conditions. A Phase I trial, illustrated the potential of the compound to relieve visceral pain through a neuronal cross-talk mechanism mediated by the GC-C pathways, setting a foundation to test the cross-talk hypothesis in humans.
While urology covers a wide spectrum of care for both men and women, at Baylor St. Luke’s we are proud to offer specialized care for female patients looking for relief from a myriad of conditions that are unique to their anatomy. Our specialists are experts in identifying and creating personalized treatment plans for women seeking relief from conditions such as pelvic organ prolapse and urinary incontinence.
With the addition of Rotimi Nettey, M.D., M.H.S., Baylor St. Luke’s has expanded it care options for women with a specialized focus in pelvic floor health, pelvic organ prolapse, uterine sparing approaches, vaginal reconstruction, genitourinary and vaginal fistulae.
“Female pelvic medicine for a lot of patients can seem quite nebulous and vague,” says Dr. Rotimi Nettey. “Women have a lot of conditions, especially after childbirth such as incontinence, prolapse or sexual dysfunction, or complications such as UTI’s or pain. This is a home for any woman suffering from these conditions to be able to benefit from specialty care that can vary anywhere from medications to surgical interventions, and even working with a physical therapist. For a long time, women never came to the forefront in terms of seeking care for these quality-of-life issues that we treat as female pelvic medicine specialist. Women were either overwhelmed with their duties, whether it was taking care of their family or economic concerns. Now we are seeing more women coming forward with conditions that we’re happy to treat.”
